Introduction
Acne is a common skin condition that affects millions of people worldwide, particularly during puberty, but it can also persist into adulthood. Among the various forms of acne, hormonal acne nodules are one of the most severe and often the most difficult to treat. These large, painful, and deeply inflamed cystic acne lesions, known as nodules, can cause significant discomfort and scarring if not properly addressed. While there are multiple treatment options available, one that stands out for its effectiveness in managing these giant inflammatory nodules is Incision and Drainage (I&D).
This article will explore the ins and outs of treating giant inflammatory hormonal acne nodules through I&D, including what the procedure entails, how it helps, recovery tips, and other important considerations for those suffering from this form of acne.
Understanding Hormonal Acne Nodules
Hormonal acne nodules are a type of cystic acne that typically form deep within the skin’s layers. They are larger and more painful than other acne types like blackheads or whiteheads. This form of acne is often linked to fluctuations in hormone levels, particularly during puberty, menstruation, pregnancy, and conditions like polycystic ovarian syndrome (PCOS).
These nodules appear as hard, raised bumps under the skin, and they can be tender to the touch. Unlike pustules or papules, which have visible openings, hormonal acne nodules do not come to a head and often require medical intervention to resolve. Due to their deep location, they can lead to scarring if not effectively treated.

What is Incision and Drainage (I&D)?
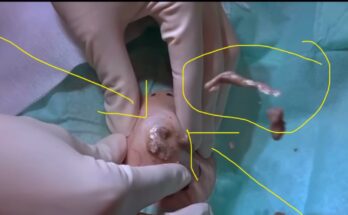
Incision and Drainage (I&D) is a surgical procedure commonly used to treat large, painful cysts or abscesses, including those caused by acne. The process involves making a small incision in the skin to release the contents of the cyst, including pus and excess fluid. By draining the cyst, the pressure and inflammation associated with the nodule are alleviated, providing relief from pain and preventing further complications.
In the context of hormonal acne nodules, I&D can be an effective method to speed up the healing process, reduce inflammation, and minimize scarring when done correctly. This procedure is typically performed by a dermatologist or a trained medical professional.

Indications for I&D in Acne Nodules
While many hormonal acne nodules will resolve with topical or oral treatments, I&D is recommended when:
- The Nodule is Large and Painful: When the acne nodule is too large and painful to heal on its own, I&D can help drain the fluid and reduce discomfort.
- No Response to Other Treatments: If topical treatments, oral antibiotics, or oral retinoids do not bring relief, I&D may be the next step.
- Risk of Scarring: Draining the nodule early may reduce the chances of long-term scarring.
- Significant Inflammation: For cystic nodules with extensive swelling, I&D can alleviate the pressure and minimize the risk of further tissue damage.

The Incision and Drainage Procedure for Acne Nodules
The I&D procedure for acne nodules is typically straightforward but requires a trained professional to ensure safety and effectiveness. Here’s a step-by-step breakdown of what you can expect during the procedure:
- Consultation and Evaluation: The process begins with a consultation, where the dermatologist assesses the severity of the acne nodules and determines if I&D is the right treatment. If deemed necessary, a treatment plan will be outlined.
- Preparation and Anesthesia: Prior to the procedure, the area around the nodule will be cleaned thoroughly to prevent infection. A local anesthetic is applied to numb the area to minimize discomfort during the procedure.
- Making the Incision: Once the area is numb, the dermatologist will make a small incision at the apex of the nodule. This incision is usually about 1-2 mm long, just enough to allow the cyst to drain.
- Drainage: After making the incision, the cyst contents (pus, sebum, and other debris) are gently squeezed out. This relieves the pressure and reduces inflammation.
- Cleaning and Closing: The area is cleaned again, and in some cases, a small drain may be placed to ensure that any remaining fluid can continue to drain out. In most cases, the incision is left open to heal naturally, but in rare cases, stitches may be used.
- Post-Procedure Care: After the procedure, the dermatologist will provide guidelines for caring for the incision site to prevent infection. This may include applying topical antibiotics, avoiding touching the area, and following up for checkups if necessary.

Benefits of Incision and Drainage for Acne Nodules
The main advantage of I&D for treating hormonal acne nodules is its ability to:
- Alleviate Pain and Swelling: By draining the contents of the nodule, the pressure and inflammation are significantly reduced, leading to pain relief.
- Speed Up Healing: I&D helps the nodule heal faster compared to waiting for it to resolve on its own.
- Prevent Scarring: Early drainage can reduce the chances of scarring, which is particularly important for individuals with sensitive skin or those prone to post-inflammatory hyperpigmentation.
- Effective in Resistant Cases: For nodules that are unresponsive to traditional acne treatments like topical creams or oral antibiotics, I&D can provide a faster and more direct solution.

Recovery After Incision and Drainage
While I&D is a minimally invasive procedure, proper post-care is essential for optimal recovery. Here’s what you can expect during the healing process:
- Initial Healing: The incision site will be sore for a few days following the procedure. Swelling should subside within a week, though redness may persist longer.
- Avoiding Infection: The incision must be kept clean and dry to prevent infection. Your dermatologist may recommend a topical antibiotic ointment to help prevent bacterial growth.
- Post-Procedure Instructions: It’s essential to avoid squeezing or picking at the treated area, as this can lead to complications such as re-infection or further scarring.
- Follow-up Appointments: Depending on the severity of the nodule, a follow-up appointment may be scheduled to ensure the area is healing properly.
Alternative Treatments for Hormonal Acne Nodules
While I&D is a highly effective treatment, there are other options for managing hormonal acne nodules. These include:
- Topical Treatments: Over-the-counter creams and gels containing benzoyl peroxide, salicylic acid, or retinoids can help reduce inflammation and prevent future breakouts.
- Oral Medications: For more severe cases, oral antibiotics, hormonal treatments (such as birth control pills), or oral retinoids (such as isotretinoin) may be prescribed to control acne.
- Steroid Injections: In some cases, corticosteroid injections may be used to quickly reduce inflammation and shrink large acne nodules.
- Laser Therapy: Lasers can be used to target and reduce the size of cystic acne nodules, promoting healing and minimizing scarring.
- Light and Chemical Peels: Light therapy and chemical peels may be used as adjunctive treatments to manage acne and improve skin texture.
When to Seek Professional Help
If you are dealing with persistent hormonal acne nodules that are not responding to at-home treatments, it’s important to consult with a dermatologist. Early intervention can prevent further complications such as scarring, skin infections, or prolonged discomfort.
Conclusion
Giant inflammatory hormonal acne nodules can be a frustrating and painful condition, but with the right treatment approach, relief is possible. Incision and Drainage (I&D) offers an effective way to manage these stubborn cysts, helping to alleviate pain, speed up healing, and reduce the risk of scarring. When combined with other acne management strategies, I&D can play a vital role in controlling severe acne and improving overall skin health. If you are struggling with hormonal acne nodules, consult with a dermatologist to explore the best treatment options for you.